| Text |
In
light of the success of the statin drugs, interest in preventive cardiology
has shifted to new frontiers of pharmacologic intervention: defining optimal
levels of low-density lipoprotein (LDL) cholesterol, inhibiting cholesterol
absorption, addressing the inflammatory component of atherosclerosis,
and increasing the levels of protective high-density lipoprotein (HDL)
cholesterol. This last approach attracted attention last year when it
was reported that a new drug, torcetrapib, could substantially increase
levels of HDL cholesterol by inhibiting cholesteryl ester transfer protein.(1)
The drug was heralded as a novel weapon against heart disease that could
be an important clinical tool if its effect on lipids actually reduces
the rate of clinical events. Subsequent studies reported in March confirmed
the drug's capacity to increase HDL cholesterol markedly.(2) Pfizer, which
holds the patent on torcetrapib, is launching several studies to assess
the clinical outcomes of treatment with the drug. One study, scheduled
to be completed next year, will evaluate the drug's effect on atherosclerotic
plaque, as measured by intravascular ultrasonography. In a second trial,
investigators will study 13,000 patients over a period of five years to
measure rates of myocardial infarction and stroke.
Enthusiasm about this potentially important new therapeutic tool has been
tempered by concern about how the company will study and market the drug.
Pfizer's trials will study torcetrapib only in combination with the company's
widely used atorvastatin (Lipitor), the best-selling drug in the world

Total Pfizer
Revenues from Lipitor, 1999–2005.
The figure for 2005 is extrapolated from first-quarter revenues. Data
are from Pfizer.
Sales
of Lipitor account for about half of Pfizer's annual profits; the company's
patent is due to expire in 2010. Because of this study design, the Food
and Drug Administration (FDA) will be presented only with data on the
torcetrapib–Lipitor combination as compared with Lipitor alone. If
the studies show that the combination is more effective than statin monotherapy,
the FDA is likely to approve torcetrapib for use only in a combination
product that includes Lipitor — not for separate use or use with
another company's statin or with a generic statin — because the only
efficacy trial data presented to it will be based on the combination tablet.
Such approval would make it impossible for physicians to prescribe the
new agent with any other statin — or even with generic atorvastatin
when it becomes available in five years.
Normally, antitrust laws would prohibit a manufacturer from offering a
drug only when "bundled" with another one of its products. It
appears that Pfizer will avoid such antitrust prohibitions by having the
FDA do its bundling for it. The FDA's acceptance of the proposed trial
designs in effect acknowledges that since the new drug is Pfizer's intellectual
property, the company's research plans are subject only to its own corporate
prerogative. These studies will enroll thousands of patients who are at
risk for cardiovascular disease, cost Pfizer millions of dollars, and
go on for years. But when they are completed, clinicians, patients, payers,
and regulators will still not know how well this important new approach
to atherosclerosis performs in combination with any risk-modifying approaches
other than Lipitor. Pfizer's position is that it invested in the development
of torcetrapib and is paying for its evaluation, so it can study and market
the resulting product however it sees fit. As with other costly new drugs,
however, research leading to the product's development was also supported
by the National Institutes of Health (NIH).(1,3)
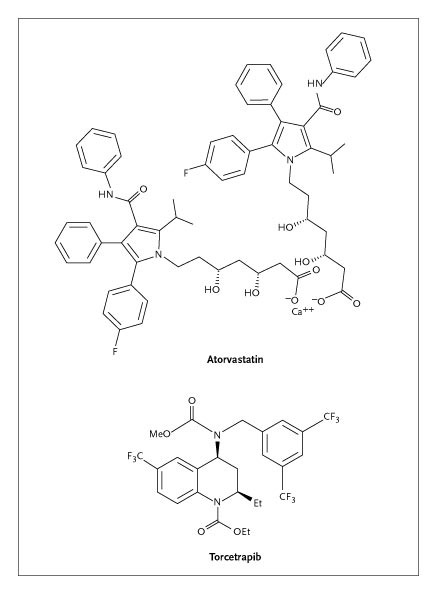
Molecular Structure
of Atorvastatin and Torcetrapib.
High cost will be the most prominent downside of the FDA-sanctioned yoking
of the two brand-name drugs. But there will be clinical problems as well:
patients who cannot tolerate (or afford) Lipitor will have no way of obtaining
torcetrapib for use with another statin that may be better for them. Physicians
who want to raise a patient's level of HDL cholesterol — but who
do not want to be forced to use Lipitor — will not have access to
torcetrapib.
Other research options would have been feasible. Although it makes sense
initially to test the additive effects of torcetrapib plus statins over
statins alone, a target level of LDL cholesterol could have been set for
the trial, with study participants randomly assigned to receive one of
several statins — a design that would have produced more generalizable
findings. In another scenario, participating clinicians could have reached
a target LDL level using the statin of their choice, with patients randomly
assigned to receive either torcetrapib or placebo in addition. The FDA
often discusses the design of preapproval studies with manufacturers and
could have tried to convince Pfizer to implement a study design geared
toward better protection of the interests of science, patients, and even
payers. But if such discussions took place, they did not succeed. This
may have been the result of the FDA's fear of litigation by the manufacturer,
since the owner of a new drug has the legal (although perhaps not the
moral) right to conduct its preapproval clinical studies as it sees fit.
The next test for the FDA will come in its response to the results of
these trials. What if the combination therapy does reduce the rate of
cardiovascular events or atherosclerotic progression better than atorvastatin
monotherapy? In principle, the FDA could approve torcetrapib for use in
combination with Lipitor, as a single agent for use with other statins,
or even alone in uncommon situations. But Pfizer is likely to request
approval only for the fixed combination, arguing that this is the sole
use of torcetrapib for which adequate trial data are available. The FDA
would have to muster uncharacteristic regulatory courage to persuade the
company to market the new drug in more than one form; the agency is unlikely
to do so and may lack the legal authority. Even if the FDA took such a
stand, it could find its options limited by the design of the preapproval
research. And in the end, whatever the FDA decided and regardless of the
role of public funds in the early development and evaluation of inhibition
of cholesteryl ester transfer protein to raise HDL cholesterol, Pfizer,
as the owner of the new compound, could still choose to make it available
only in combination with Lipitor.
The torcetrapib controversy brings several long-standing questions about
clinical drug research into sharp focus. In the 1990s, as pharmaceutical
companies became the most profitable industry group in the nation, their
annual research expenditures began to exceed the entire budget of the
NIH. Those profits and expenditures did not result in an impressive increase
in the rate of discovery of important new drugs by most of the large firms,
raising troubling questions about the supposed link between huge cash
flows and genuine innovation. Nonetheless, these shifting economic realities
helped entrench the dominance of pharmaceutical companies over the research
agenda for therapeutics. Growing deficits in the federal budget now place
considerable pressure on publicly funded medical research, which will
further limit the ability and willingness of the NIH to support applied
studies of drug efficacy and safety in the future. Thus, the scientific
questions that are asked in both domains will increasingly be defined
by the pharmaceutical industry.(4)
The torcetrapib–Lipitor bundling studies illustrate where this trend
can lead. The current trial designs may not optimally meet the scientific
needs of prescribers, the clinical needs of patients, the economic needs
of payers, or the regulatory needs of policymakers. But they superbly
meet the business needs of the sponsor — to create new knowledge
in a way that will protect the market share of the largest drug company's
most important product. A more science-based or patient-centered research
design would not have accomplished this goal as well; indeed, any Pfizer
official who signed off on such a study might be accused of compromising
his or her fiduciary responsibility to the company's shareholders.
This is the predictable consequence of an industry-driven approach to
defining the nation's drug-research agenda. But another vision is possible,
and it would reduce rather than increase public expenditures. Well-targeted
federally funded medication trials can more than pay for themselves; examples
to date include NIH-supported studies of estrogen replacement and of medications
for hypertension, which provided important insights into the risks, benefits,
and optimal use of these therapies. These needed insights can improve
care and save the nation billions in drug expenditures.(5) For instance,
if a moderate-size NIH-funded clinical trial of the cardiovascular risks
of coxibs had been performed in 2000 and 2001, most of the $2.5 billion
per year — about $1 billion annually from public coffers — that
was spent on rofecoxib (Vioxx) might have been saved. Other clinical examples
abound.
The torcetrapib story suggests that we have become too dependent on manufacturers
as the predominant source of our scientific knowledge about the effects
of medications. As Medicare prepares for an increasingly unaffordable
drug benefit, the best way to contain that public expenditure will be
to commit a small fraction of those funds to support such public-interest
drug trials, fairly comparing competing therapies (especially costly new
ones) with clinically realistic alternatives. With pharmaceutical costs
increasing faster than most other health care expenditures, the nation
requires studies that will meet the needs of evidence-based prescribing
and not just the needs of the pharmaceutical industry. It is not a question
of whether we can afford to pay for our own drug trials; it is increasingly
evident that we cannot afford not to do so.
Source
Information Dr. Avorn is a professor of medicine at Harvard Medical School
and chief of the Division of Pharmacoepidemiology and Pharmacoeconomics
at Brigham and Women's Hospital — both in Boston.
References
1) Brousseau ME, Schaefer EJ, Wolfe ML, et al. Effects of an inhibitor
of cholesteryl ester transfer protein on HDL cholesterol. N Engl J Med
2004;350:1505-1515.
2) Davidson M, McKenney J, Revkin J, Shear C. Efficacy and safety of a
novel cholesteryl ester transfer protein inhibitor torcetrapib when administered
with and without atorvastatin to subjects with a low level of high-density
lipoprotein cholesterol. J Am Coll Cardiol 2005;45:Suppl 1:394A-394A.
3) Brousseau MF, Diffenderfer MR, Millar JS, et al. Effects of cholesteryl
ester transfer protein inhibition on high-density lipoprotein subspecies,
apolipoprotein A-I metabolism, and fecal sterol excretion. Arterioscler
Thromb Vasc Biol 2005;25:1057-1064.
4) Avorn J. Powerful medicines: the benefits, risks, and costs of prescription
drugs. New York: Alfred A. Knopf, 2004.
5) Fischer MA, Avorn J. Economic implications of evidence-based prescribing
for hypertension: can better care cost less? JAMA 2004;291:1850-1856.
|
