| Text |
These
are trying times for patients with chronic musculoskeletal pain. Worrying
data about the drugs they regularly use keep emerging. In September 2004
rofecoxib (Vioxx) was withdrawn by Merck after the adenomatous polyp prevention
on Vioxx (APPROVe)(1) trial showed an increase in major cardiovascular
events in patients with a history of colorectal adenomas who were randomised
to receive Vioxx, compared with those in the placebo group.w1 Rofecoxib
had been marketed as the non-steroidal anti-inflammatory drug (NSAID)
of choice because selective inhibition of the isoform 2 of the cyclooxygenase
(COX 2) enzyme made it highly effective but free from gastrointestinal
toxicity.
More unwelcome data from placebo controlled trials of rofecoxib's competitors
followed: valdecoxib (Bextra, Pfizer) taken after coronary artery bypass
grafting was shown to be associated with an increased incidence of cardiovascular
events(2); and the adenoma prevention with celecoxib (APC) trial(3) reported
an increased risk of cardiovascular events associated with use of celecoxib
(Celebrex, Pfizer), a drug known to be less selective for COX 2 than rofecoxib
or valdecoxib.(4) A small increase in the risk of myocardial infarction
was also observed for the highly selective lumiracoxib (Prexige, Novartis).(5)
No data on the cardiovascular safety of etoricoxib (Arcoxia, MSD) from
large trials have been published so far, but no news is no longer good
news: patients and doctors are anxious to know whether cardiotoxicity
is a class effect applicable to any COX 2 inhibitor, or even to NSAIDs
in general.
In this week's BMJ two observational studies address this question. A
retrospective cohort study (BMJ_2005_330_1370)(6)
in patients with congestive heart failure found lower mortality in patients
treated with celecoxib than with rofecoxib or traditional NSAIDs. A case-control
study nested in a UK general practice database (BMJ_2005_330_1366)(7)
found a similar risk of myocardial infarction for celecoxib, rofecoxib,
ibuprofen and naproxen, but a somewhat higher risk with diclofenac.
We believe that these results should be interpreted with caution. For
example, the similar risk of myocardial infarction for naproxen and rofecoxib
found in the case-control study(7) is incompatible with the trial data(8)
and could be explained by confounding by indication if patients with a
history of heart disease were more likely to receive naproxen than rofecoxib
or other NSAIDs. The quality of the data on cardiovascular risk factors
and other potential confounders was poor in both studies, and the ability
to control for confounding therefore limited. For example, information
on smoking was unrecorded in 13% of cases and 20% of controls in the case-control
study(7) and entirely unavailable in the retrospective cohort study.(6)
What are the alternatives? We have argued that all unbiased data on serious
adverse events from clinical trials should be made available to independent
researchers and the public and analysed in a timely fashion.(9) Indeed,
in the case of rofecoxib, cumulative meta-analysis of clinical trial data
showed that an increased risk of myocardial infarction was evident from
2000 onwards.(8) Similar analyses are now required for the other COX 2
inhibitors.
The US Food and Drug Administration (FDA) and other licensing authorities
are an important source of relevant data. The FDA reviews clinical trials
worldwide before approval and labelling, and again before relabelling
of approved drugs. As part of the 1966 Freedom of Information Act, the
agency is required to make available its reports on all drugs that are
approved. Unfortunately, these reports are not as useful as they could
be. We found that the criteria for including trials in reports were often
unclear. For example, only 16 out of at least 27 trials of celecoxib that
were performed up to 2002 in patients with musculoskeletal pain were included
in the relevant reports. In any event, reporting on study characteristics
and adverse events was not always transparent, and complete data on cardiovascular
safety were available for only three trials. In the case of valdecoxib,
we found that many pages and paragraphs had been deleted because they
contained "trade secret and/or confidential information that is not
disclosable" (figure).w2
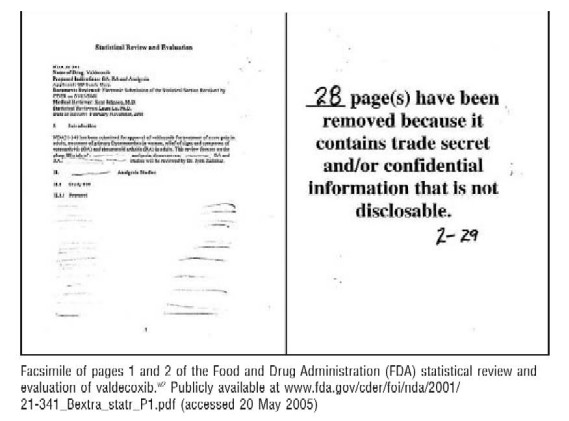
Facsimile
of pages 1 and 2 of the Food and Drug Administration (FDA) statistical
review and evaluation of valdecoxib.w2 Publicly available at
www.fda.gov/cder/foi/nda/2001/21-341_Bextra_statr_P1.pdf
Surely,
the protection of the public's health justifies full access to the safety
data submitted by industry to the FDA and other drug licensing authorities,
and mandates transparent reporting on harms, in accordance with international
guidelines.(10) Meta-analyses of adverse events might not resolve controversies,
but will help decision making about issues such as the need for additional
trials.
Observational
studies "simply cannot test definitely whether there are small to
moderate risks or benefits of a class of drugs when the factors associated
with prescription of a particular drug are difficult to control and perhaps
even uncontrollable."(11) This statement referred to postulated adverse
events of calcium antagonists in the treatment of hypertension, a controversy
finally resolved by large pragmatic trials, including the seminal antihypertensive
and lipid lowering treatment to prevent heart attack trial (ALLHAT).(12)
Such large trials might be required, ultimately, to establish the best
and safest treatment for patients with musculoskeletal pain.
Peter
Jüni, Stephan Reichenbach, Matthias Egger
References
1) Bresalier RS, Sandler RS, Quan H, Bolognese JA, Oxenius B, Horgan K,
et al. Cardiovascular events associated with rofecoxib in a colorectal
adenoma chemoprevention trial. N Engl J Med 2005;352: 1092-102.
2) Nussmeier NA, Whelton AA, Brown MT, Langford RM, Hoeft A, Parlow JL,
et al. Complications of the COX-2 inhibitors parecoxib and valdecoxib
after cardiac surgery. N Engl J Med 2005;352: 1081-91.
3) Solomon SD, McMurray JJ, Pfeffer MA, Wittes J, Fowler R, Finn P, et
al. Cardiovascular risk associated with celecoxib in a clinical trial
for colorectal adenoma prevention. N Engl J Med 2005;352: 1071-80.
4) Warner TD, Mitchell JA. Cyclooxygenases: new forms, new inhibitors,
and lessons from the clinic. Faseb J 2004;18: 790-804.
5) Farkouh ME, Kirshner H, Harrington RA, Ruland S, Verheugt FW, Schnitzer
TJ, et al. Comparison of lumiracoxib with naproxen and ibuprofen in the
Therapeutic Arthritis Research and Gastrointestinal Event Trial (TARGET),
cardiovascular outcomes: randomised controlled trial. Lancet 2004;364:
675-84.
6) Hudson M, Richard H, Pilote L. Differences in outcomes of patients
with congestive heart failure prescribed celecoxib, rofecoxib, or non-steroidal
anti-inflammatory drugs: population based study. BMJ 2005;300: 1370-3.
7) Hippisley-Cox J, Coupland C. Risk of myocardial infarction in patients
taking cyclo-oxygenase-2 inhibitors or conventional non-steroidal anti-inflammatory
drugs: population based nested case-control analysis. BMJ 2005;300: 1366-9.
8) Jüni P, Nartey L, Reichenbach S, Sterchi R, Dieppe PA, Egger M.
Risk of cardiovascular events and rofecoxib: cumulative meta-analysis.
Lancet 2004;364: 2021-9.
9) Dieppe PA, Ebrahim S, Martin RM, Jüni P. Lessons from the withdrawal
of rofecoxib. Patients would be safer if drug companies disclosed adverse
events before licensing. BMJ 2004;329: 867-8.
10) Ioannidis JP, Evans SJ, Gotzsche PC, O'Neill RT, Altman DG, Schulz
K, et al. Better reporting of harms in randomized trials: an extension
of the CONSORT statement. Ann Intern Med 2004;141: 781-8
11) Buring JE, Glynn RJ, Hennekens CH. Calcium channel blockers and myocardial
infarction. A hypothesis formulated but not yet tested. JAMA 1995;274:
654-5
12) Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting
enzyme inhibitor or calcium channel blocker vs diuretic: the antihypertensive
and lipid-lowering treatment to prevent heart attack trial (ALLHAT). JAMA
2002;288: 2981-97
|
